The Next Generation Of Vaccines
The Power Of Vaccines
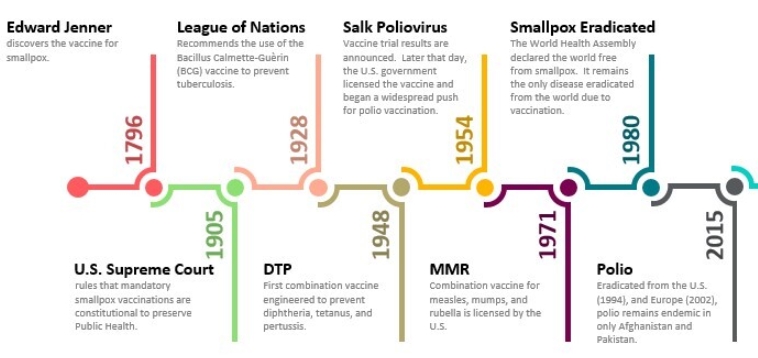
Since their invention in the 19th century, vaccines have been a massive healthcare revolution. In part, they drastically reduced mortality from deadly diseases, with no less than 154 million lives saved over the past 50 years, according to the World Health Organization (WHO).
İçindekiler
Vaccines have also entirely eradicated the terrible disease that was smallpox, which is estimated to have killed 500 million people in the last 100 years of its existence.
The next on the chopping block might be polio, with the last pockets of endemic polio in Pakistan and Afghanistan. Polio used to kill half a million people every year before vaccination.
Source: Source: Delaware Journal Of Public Health
And, of course, the recent pandemic has seen vaccine and anti-vaccine movements at the forefront of the public discourse, with mRNA vaccine technology making a spectacular entry into the market and public awareness.
Despite these successes, infectious diseases still account for around 40% of all recorded deaths in the world. In part, this is due to insufficient vaccination coverage in poor developing countries, but it is also due to some diseases still resisting the effort to develop vaccines against them.
This might change thanks to many new technologies converging into creating a new generation of vaccines.

Source: Phrma
How Vaccines Work
The base principle of a vaccine is to “train” the immune system before it encounters a dangerous disease caused by a virus or bacteria (the pathogen).
This works by presenting to the body either part of the pathogenic (“disease-causing”) bacteria or virus (the antigen) or the full pathogen, which is either killed or weakened so it cannot cause the disease.
When it is done, the body”s immune system starts developing proteins called antibodies. These antibodies “click” to specific parts of the pathogen or antigen, recognizing it in the same way a key and lock work.

Source: Cusabio
It is the specificity of the antigen-antibody interaction that allows for the antibody to neutralize the pathogen and protect the person against the disease.
You can also watch this 3min video animating these base principles of vaccination:
For some diseases, like smallpox, this worked so well that we managed to fully exterminate the disease.
But others are trickier. Here are some of the methods pathogens can use to escape vaccines and the immune system:
- Highly variable antigens. This is the strategy used by the flu and common cold viruses, with so many variants that every year, the seasonal flu is a “new” disease from a vaccine and immune system point of view.
- Low concentration and hiding. Some diseases are very good at hiding away from the immune system. They usually cause chronic diseases, but if the immune system cannot find them, vaccination is less useful or might not work at all.
- Neutralize the Immune system. Most notably, this is how HIV works, directly attacking the antibody-producing systems of the body.
- Attack quickly. Some diseases strike so quickly that the body does not have the time to react and produce enough antibodies in time. This is notably a problem with very aggressive & deadly diseases like Ebola.
The Next Targets For Vaccination
Chronic infections
As mentioned above, a segment of diseases that have overall resisted efforts to develop vaccines are chronic diseases.
Because these diseases evolved to create an infection that stays below a threshold that would trigger an efficient immune response, it is hard to create a vaccine that works. This includes a few major global killers.
Malaria
There were 249 million cases of malaria in 2022, causing around 600,000 deaths per year, with most of them children under 5 years old. This is also a very debilitating disease, leading to missed school and work days, loss of energy, income, and economic opportunities, altogether a cause of and made worse by poor economic conditions.
For example, in Mozambique, malaria was the cause of 45% of outpatient consultations and 24% of hospital admissions in 2015.
“The median household cost associated with uncomplicated malaria represents between 10% (US$ 1.63) and 21% (US$ 3.46) of the monthly expenditure of a family in Zambézia, while the cost of a severe case (US$ 64.90 and US$ 81.08) exceeds the mean monthly expenditure per capita by more than three times.”
Malaria Journal
Malaria is caused by a parasite that hides in the patient’s liver and is transmitted through mosquito bites. It also has more than 60 variable antigen genes and switches between them to hide further from the immune system.
Until recently, a malaria vaccine has been difficult to develop, leading to the main effort to control the diseases focused on targeting the mosquitoes instead. Drugs are also a possibility, but the parasite tends to develop resistance against previously efficient molecules.
Finally Available Vaccines
In 2021, the WHO recommended for widespread use of the RTS, a malaria vaccine for children in affected areas, produced by pharmaceutical giant GSK. In 2023, a second malaria vaccine (R21/Matrix-M), created by the University of Oxford, was approved.
Both approved malaria vaccines do not fully avoid the disease, but radically reduce the severity of the symptoms and the risk of death. These vaccines use artificial proteins and virus-like particles.
Among the candidates for new, more efficient vaccines are the PfSPZ vaccine in development by Sanaria. It is now in Phase 2 of clinical trials and uses a genetically modified version of the whole parasite.
“Only Sanaria’s P. falciparum sporozoite vaccines have achieved >90% vaccine efficacy against controlled human malaria infections”
Sanaria
HIV/AIDS
HIV, the virus causing AIDS, was infecting 39 million people in 2022, causing 630,000 deaths. While patients can see lower mortality and higher quality of life by using anti-HIV drugs, a cure and eradication of the disease will likely require a vaccine.
By attacking the CD4 cells, a part of the immune system, the virus manages to avoid detection until it is too late.

Source: Delaware Journal Of Public Health
A vaccine has been very difficult to develop, and it is still unclear what will work.
Among the notable efforts and potential cures in development are:
Others
It would be too long to cover all the existing vaccine initiatives. You can read more about it in this 11-page report.
Among the other important diseases with active efforts made to develop a vaccine against them are:
- Dengue
- Hookworm
- Leishmaniasis
- Cytomegalovirus (herpes)
- Lyme disease
- Shingles
Aggressive infections
New diseases and aggressive patterns of infection can overwhelm the immune system and lead to very high death rates in infected patients.
One example is Ebola and other hemorrhagic fevers, with death rates in the 30-50%. There are currently 2 Ebola vaccines, Merck’s Ervebo approved in 2019, and Johnson & Johnson’s Zabdeno+Mvabea.
Of course, another example is coronavirus, the cause of the COVID-19 pandemic, but also of the previous deadly outbreaks of Middle East respiratory syndrome coronavirus (MERS-CoV) and 2002-2004 Severe acute respiratory syndrome (SARS).
New Vaccine Technology
Previous generations of vaccines were based on a few techniques, like using a weakened part of the virus/bacteria, a dead full-version of it, just fragments, or more recently the antigen expressed into another vector through genetic modification.
Modern biosciences are now coming with many new potential modes of vaccination.
mRNA Vaccines
Widely promoted and very quickly adopted because of the COVID-19 pandemic, mRNA vaccines have a powerful advantage over traditional vaccines.
Instead of slowly finding how to safely inactivate a virus, or how to efficiently modify another vector, it can directly “program” a cure in just 3-4 weeks. This is because the mRNA code can be directly written once the targeted virus genome is known, something that was achieved in the very first week of Covid-19 identification.
Other COVID vaccines existed during the pandemic, but the quick development cycle of mRNA vaccines made it the perfect solution for a novel disease.
More mRNA vaccines are now in development, especially by the 2 companies that benefited the most from the mRNA vaccines’ sales during the pandemic.
- Moderna is developing mRNA vaccines for coronavirus, the flu, as well as RSV, Zika, HIV, Epstein-Barr virus, Varicella zoster virus (VZV), norovirus, Lyme disease, and cytomegalovirus.
- BioNTech, the partner of Pfizer is also active, with mRNA vaccines in development covering shingles, malaria, Mpox, HSV, tuberculosis, and the flu.
Nucleic Acid Vaccines
While technically, mRNA vaccines are a sub-category of nucleic acid vaccines, the technology is broader and includes a few other potential types of vaccines.
The first one is DNA vaccines, which use a molecule of DNA instead of RNA. Over 160 different DNA vaccines are currently being tested in human clinical trials in the United States. It is estimated that 62% of these trials are devoted to cancer vaccines and 33% are applied to vaccines against human immunodeficiency virus (HIV).
Growing Vaccines In Farms
We are used to thinking of vaccines as full or parts of a virus/bacteria. Even antigen-based vaccines are produced by multiplying this antigen in unicellular organisms.
But this might change with the progress of genetic modification, with the hope to one day produce vaccine material the way we grow food.
Plant-based vaccines could be growing the vaccine component in open fields or greenhouses. This would radically reduce production costs.
The issue is that most antigens will not be produced in plants the way they would in bacteria or viruses, due to different cellular biochemistry, notably the sugars added to proteins.
A more promising field than growing vaccines in plants like corn or wheat is using microalgae. The technology is now starting to be used for animal vaccines, and the microalgae cell wall provides a pre-existing “capsule” making the vaccine edible instead of needing purification and injection
Organoparticles
Changing the fundamental technology of vaccine production is not the only way to improve vaccines.
For example, most vaccines use “adjuvants,” chemical compounds that boost the immune system. However, these can cause unwanted side effects as they stimulate ALL immune reactions, not just the ones intended by the vaccine.
Instead, a recent publication by a research team from MIT might have found a solution to increase vaccine effectiveness by using a novel type of adjuvant leveraging nanotechnology.
They used a metal-organic framework (MOF) nanoparticle, which acts as an adjuvant, boosting a specific immune reaction instead of a generalized reaction like with classical adjuvants. We discussed this discovery in more detail in our article “Boosting Efficacy of Vaccine through Metal-Organic Nanoparticles”
Mixed flu shot
A more powerful or quicker development cycle might still leave highly variable viruses like the seasonal flu free from a perfectly efficient vaccine.
This is because these vaccines target antigens that are highly variable, allowing the virus to quickly escape the acquired immunity.
Researchers are now finding that they can force the immune system to focus on other, less variable sections of the virus. We discussed how this was done by combining 80,000 mutated versions of the flu virus in our article “Flu Shots Can be Shot in the Dark – Scientists are Looking to Shed Light on a New Approach”.
Better Logistics & Delivery
Other improvements that could be made regarding vaccines are related to logistics and methods of administration. A lot of vaccination campaigns come from logistics, cold storage, the need for medical professionals to inject the vaccine, etc.
For example, Cambridge’s researchers found a way to trap viral particles in an ultrathin layer of sugar glass, allowing for storage at temperatures of up to 113°F for six months.
As discussed above, an algae-based vaccine could be delivered orally, like a vitamin pill.
Another option could be vaccine microarray patches (vaccine-MAPs), also known as microneedle patches. This injection-free option is painless and could improve both logistic challenges and compliance while making the administration of vaccines quicker.
Digital Vaccines Records
Lastly, technology could help monitor the vaccination status of individual people and the whole population. Digital records can help decision-makers design better vaccination campaigns, anticipate epidemics, and improve vaccination rates.
Non-Transmittable Diseases Vaccines
While probably not technically “vaccines,” there are many new vaccine-like treatments in development looking to prevent death by modifying the body’s chemistry or immune system.
Cancer Vaccines
As cancer is quickly becoming a larger cause of death than infectious disease worldwide, better treatments are becoming increasingly important.
Technically, some cancer vaccines already exist for cancers induced by infectious diseases, like HPV and Hepatitis B.
Another category is therapeutic cancer vaccines. They are looking to make the immune system react to cancer cells the way it would to an infectious pathogen.
This is done by inducing the immune reaction against antigens present in the cancer cells.
Already, several cancer vaccines have been approved for prostate and bladder cancer, as well as melanoma.
More are in development for almost every type of cancer, especially the ones resistant to currently available therapies, like pancreas cancer.
Anti-aging Vaccines
One possibility to fight aging is creating induced-Pluripotent Stem (iPS) cells, with massive potential to repair and rejuvenate the body’s tissues. This reprogramming could be achieved through a transient genetic reprogramming, relying on an mRNA-based method.
This method is very similar to the mRNA vaccines, except the target is not to create immunity but to temporarily modify the targeted cell.
We look at transient cellular reprogramming and other anti-aging potential technologies in our article “Aging is a Part of Life – That Doesn’t Mean We Can’t Put Up a Fight”.
Alzheimer’s Vaccine
With the population aging, Alzheimer’s is a growing public health concern.
The American company Vaxxinity reported successful phase 2 trials of UB-311, targeting toxic amyloid beta forms in the brain, which not only triggered an immune response but also demonstrated safety.
Many other potential Alzheimer’s vaccines are in trials, with others targeting the amyloid proteins, as well as targeting the tau protein, or inflammation.
Diabetes
Type-1 diabetes is an autoimmune disease where the body’s immune system targets the insulin-making cells in the pancreas. So it makes sense that a “vaccine” modulating immunity could potentially prevent this disease.
Macrogenics’ TZIELD was approved in 2022 and reduces the risk of developing type-1 diabetes. While not foolproof, this is a massive step into one day fully avoiding the disease developing or reversing the damages it causes.
Inflammation Vaccines
A vaccine targeting human cytokines, a key factor in asthma, was invented in 2023. Other “vaccines” (really monoclonal antibodies) targeting psoriasis are also in development.
Similar progress in managing inflammation and autoimmune disorders is ongoing, with many vaccine candidates targeting cytokines as well, which include:
Vaccines Companies
1. BioNTech (BTNX)
BioNTech is doubling down on the technology that forms the core of its business. The company behind the Covid mRNA vaccine sold by Pfizer is now using the money made during the pandemic to widely expand its offer.
It is now developing mRNA vaccines for shingles, tuberculosis, malaria, HIV, and the herpes virus. This makes it a leading company in the field of mRNA vaccines, with only its competitor Moderna (MRNA) developing more mRNA vaccines than BioNTech.
BioNTech is also exploring the potential of mRNA for cancer, with 12 different candidate products for cancer treatment in its pipeline.

Source: BioNTech
Finally, it also has in its R&D pipeline some cell therapies and other non-mRNA potential cancer treatments.
mRNA has been a revolution in therapy for viral infection. BioNTech is counting on mRNA being an equally massive revolution in oncology.
With a presence in the whole spectrum of mRNA vaccine potential, both for infectious diseases and for cancer, BioNTech provides investors with exposure to both.
2. Immatics
Immatics is looking to reprogram the immune system to target cancer cells, making it a leader in cancer “vaccines”, also called TCR therapies.
Two fundamental steps are required:
- picking a true cancer target that is naturally and specifically expressed at significant levels on the tumor.
- developing the right, potent TCR that specifically recognizes the selected cancer target with minimal or no cross-reactivity with healthy tissues.

Source: Immatics
The company’s R&D pipeline is split between therapies where the cells are collected for each patient (autologous) and “off-the-shelf” therapies (heterologous).
The company has established a strong line-up of partnerships, including with BMS, Moderna, and Editas.

Source: Immatics
The partnership with Moderna for a “strategic multi-platform collaboration” was established at the end of 2023.
Immatics’ products are still at an early stage but have massive potential, something clearly recognized by leaders of the industry like BMS and Moderna.
The company’s candidate therapies target melanoma and cancer in the ovaries, lungs, uterus, bladder, head & neck, as well as other types of solid cancers.
Conclusion
Vaccination has changed the world, saving hundreds of millions of lives. And it might soon have an equally large impact, potentially wiping out deadly diseases that have plagued humankind for eons.
We might also see relatively soon the emergence of new vaccine types. Some will leverage new technologies to target diseases so far not targeted by vaccines. Or to make vaccines that would be injection-free, painless, edible, cheaper, and that could be stored at room temperature.
Finally, our deepening understanding of the immune system and the mechanics of inflammation might open the way to “quasi-vaccines” preventing or curing diseases as varied as Alzheimer’s, asthma, or diabetes.